Source: Cambridge Equine Hospital
One of the most common veterinary problems seen in horses is osteoarthritis (also known as degenerative joint disease). There is no cure for this disease, as once arthritic changes have started they cannot be reversed. However, slowing progression of the disease through correct management is usually possible.
Horses with joint issues will show lameness, pain on flexion of the affected joint, or even generalised stiffness. Early signs of joint disease can be subtle, so owners must carefully monitor their horses for signs such as; joint swelling, localised heat, lameness or reduced ability to perform athletically. By the time these symptoms are noticed irreversible changes to the joint architecture may already be underway. Common joints affected include the hock, pastern, coffin, fetlock, carpal (knee) and stifle joints.
Before initiating any type of treatment it is very important to have a correct diagnosis. The source of pain needs to be identified via a thorough veterinary lameness examination. This is usually done though a combination of diagnostic anaesthesia (local anaesthetic/nerve blocks) and radiographs (x-ray). Diagnosis of the condition is essential, as if you mask the pain of a surgical lesion (e.g. a chip fracture) with medical treatments into the joint, then you can end up doing more damage. (See images below)
Once a diagnosis has been made there are usually several treatment options. For cases of mild osteoarthritis there are many nutraceuticals available as in-feed supplements or systemic drugs. Many of these work on the premise of providing building blocks of molecules that are integral in the articular cartilage or joint fluid. These may be of benefit for mild cases or the prevention of osteoarthritis. Buyer beware: There are many products on the market that have very little scientific support. Generally, the most reputable treatments (such as 4CYTE granules) include active ingredients such as chondroitin sulphate, glucosamine, and pentosan polysulfate.
So why do we treat joints via direct injection?
Direct injection of affected joints is often the ideal method of treatment as it ensures that the medication can be delivered directly to the site of action. Treatment is indicated to decrease soft tissue swelling and pain. By halting the inflammatory cascade, treatments may slow the progression of permanent osteoarthritis changes.
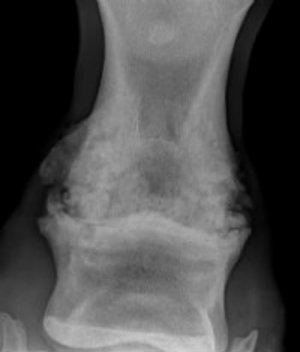
The image above is an example of severe osteoarthritis of the pastern joint that has progressed beyond the point of treatment. Note the reactive, mottled appearance to the bone around the joint, which should normally have a smooth contour. This case was attempted to be managed medically and did not respond favourably. The next option for this horse would be radical surgical intervention in the form of surgical arthrodesis (fusing the joint).
Osteochondral fragments or “bone chips” (like the one on the right) are best removed surgically as medical treatment will just mask pain and the progression of the disease. Cases like this are best managed by taking out the bone fragment via arthroscopy.
Below are the options we currently have for direct medication of joints.
Corticosteroids:
Triamcinalone is the most commonly injected corticosteroid and has been evaluated in equine research models. Several studies have shown certain corticosteroids to be protective to the joint environment if used correctly. Overuse or misuse of certain steroids may be degradative or damaging to the joint.
Hyaluronic acid (HA):
HA is normally made by the synovial membrane (within the joint). HA is responsible for the lubrication of articular cartilage and therefore is essential for normal joint mobility. Experimental evidence has shown that the highest molecular weight (thickness) of HA provides the most benefit to equine athletes. Studies have shown that HA will help decrease joint inflammation and therefore treat arthritis.
The combination of both corticosteroids and HA has been scientifically proven to have a more thorough and lasting effect than HA alone or corticosteroids alone. This is a very common treatment used by equine practitioners.
Stem Cells:
Stem cells are now being used to treat equine joint disease. These mesenchymal stem cells have been shown they do have an affinity for damaged joint tissues. Some recent studies have even shown that they can have an ability to help repair of damaged soft tissue joint structures (e.g. ligaments and menisci).
It is thought that through restabilisation of the soft tissue structure of the joint osteoarthritic changes may be slowed down or even halted. Limited clinical trials are yet to be done with large numbers of horse therefore caution is always advised when dealing with such new treatments.
PSGAG’s – Polysulfated Glycosaminoglycans:
These types of drugs are most commonly administered by intramuscular injection; however some can also be used intraarticularly. These products are primarily used as the building blocks for successful cartilage reparation. It is likely they have a positive effect on joint health when used correctly.
PRP- Platelet-rich plasma:
PRP is a common treatment of ligament and tendon injuries in horses. It releases substances that encourage tissue repair (via growth factors) and help decrease inflammation. Anecdotally PRP can resolve lameness in joints that have been unresponsive to corticosteroid treatments .This treatment is used in human medicine on conditions such as tennis elbow. It may be of great benefit in the future however research on the beneficial effect of PRP in the equine joint is still needed.
How often do joints need to be re-injected?
It really varies from horse to horse. Some horses may require a one off injection to settle down inflammation while others will require it every few months. Typically, when there is mild soreness joint therapy is indicated 2 to 3 times per year.
Consult your veterinarian each time your horse requires re-injecting as a radiograph may be required to ensure that the disease has not progressed.
Are there any risks of joint injections?
Therapeutic joint injections should not be used as a preventive measure where there is no existing problem. This is because joint injections are not without risk. Such problems that can be encountered include infection, joint “flare”, masking of lameness, and overuse of steroids. If you are not familiar with the procedure of injecting joints, your vet will talk you through the possible complications, and what can be done to reduce the risk.
Joint injections and medications for osteoarthritis are not miracle cures. It is essential that a correct diagnosis is established prior to any type of treatment. Joint therapy is just one of the many tools available for prolonging your horse’s athletic career.






